Glossary
The below definitions include variables in the database as well as global health terms that arise frequently in global health cost-effectiveness analyses.
Age-Weighting: Age-weighting can assign a higher priority to specific periods of each population member’s life. For example, age weighting can prioritize health for people during their most economically productive years over health during their childhood and at later ages. GBD 1990 and 2004 recommended age weights that assign weights that differ by age, while GBD 2001-2002 and 2010 recommended uniform age weighting. Uniform age-weighting means that all ages are weighted the same, thus no age is preferred (Murray et al. 1996; WHO: Disability weights, discounting and age weighting of DALYs).
Cost-effectiveness Acceptability Curve : A cost-effectiveness acceptability curve (CEAC) conveys how likely it is that an intervention’s cost-effectiveness ratio is less than (i.e., is more favorable than) various threshold values. More specifically, the CEAC plots the willingness-to-pay (WTP) value to avert a DALY on the horizontal axis against the probability that the cost-effectiveness ratio falls below that WTP value on the vertical axis.
Comparator : The alternative intervention to which the intervention of interest is compared. The cost-effectiveness ratio is computed using the incremental cost of the incremental benefit of the intervention of interest relative to the comparator’s cost and health benefit.
Cost-Effectiveness Threshold: A quantity that represents the subjective monetary value of averting one DALY. Analyses compare estimated cost-effectiveness ratios to this threshold to determine if intervention represents good value. The World Health Organization (WHO) has suggested that an appropriate cost-effectiveness threshold in a country might be 1 or 3 times the gross domestic product (GDP), though WHO is reviewing alternative estimation methods to inform thresholds
Cost-saving: An intervention is considered “cost saving” if, relative to the comparator, it reduces total health costs, and if it improves health, or at least does not make health worse.
Country of Study: The country (or countries) for which the study and results are applicable.
Currency and Year: The currency (and year of that currency) used in the study to quantify monetary costs and savings.
Disability-Adjusted Life Year (DALY) : The WHO defines 1 disability adjusted life year (DALY) as equivalent to 1 year of healthy life lost. DALYs are calculated as the sum of years of healthy life lost due to disability (YLD) and years of life lost (YLL) due to mortality (WHO 2003).
Years of life lost is YLL = N X L, where N is number of deaths, and L is the standard life expectancy at age of death in years.
Years lost due to disability is YLD = P X DW , where P is the condition’s proportion of the population with the condition, and DW is the condition’s disability weight.
Disability weight: A disability weight is a measure of the decline in health due to a disease. The disability weight is measured on a scale of 0 (healthy) to 1 (dead). Disability weights are used to calculate YLD (Years Lost due to Disability) and hence to quantify a disability impact (WHO: Disability weights, discounting and age weighting of DALYs). The YLD is combined with YLL to estimated Disability-Adjusted Life Years (DALYs).
Discount Rate: The amount by which the value of a cost or benefit decreases when it is deferred for an additional year into the future. The discount rate reflects the typical preference to accrue benefits sooner rather than later, and to defer costs. Using the discount rate, it is possible to convert all future benefits and costs to their corresponding present value equivalents. That conversion makes it possible to sum the values of events that take place at different times and determine the present value of benefits and costs.
For instance, the present value (PV) of disability-adjusted life years averted (DALYs) occurring n years in the future is calculated as:
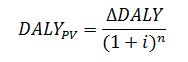
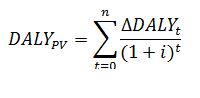
where i is the annual discount rate. For interventions that affect DALYs averted over more than a single year, the present value can be calculated by summing over all affected years. Mathematically, this can be written as:
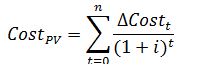
where t indicates the number of years in the future. The present value of a change in costs occurring over n future years can be calculated in a similar manner. That is:
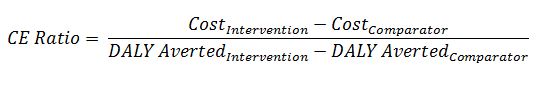
The cost-effectiveness ratio is:
.
A discount rate is typically not applied if an assessment’s time horizon is less than a year (Gold et al. 1996).
Disease Classification: A category to which the primary disease addressed by the intervention and the comparator is assigned. Categorization schemes include ICD-10 and the Global Burden of Disease Classification system (Murray et al. 2012).
Dominant : An intervention is dominant if it costs less than the comparator and is at least as effective. In the GHCEAR, categorization scheme, “dominant” is equivalent to “cost saving”.
Dominated: The intervention costs more than the comparator and is no more effective.
Environmental Augmentation : An addition to the built environment designed to promote better health outcomes (e.g. sewage systems) (Merriam-Webster.com).
Environmental Remediation: The removal of pollution, toxins, and contaminants from the environment in order to promote improved health outcomes (Merriam-Webster.com).
GAVI : The Global Alliance for Vaccines and Immunizations (GAVI) was founded in 2000. GAVI brings together UNICEF, the World Health Organization, the World Bank, the Bill and Melinda Gates Foundation, the vaccine industry, and other private and public partners in order to improve access to immunizations in the world’s poorest countries (GAVI.org).
GAVI Eligible Countries : Countries that can apply to GAVI for support in purchasing vaccines for their country. There are currently (as of 2016) 54 countries that are eligible for GAVI support. To be eligible for GAVI support, countries must have a “GNI (gross national income) of less than or equal to US $1,580 on average over the last three years” (GAVI.org).
Global Burden of Disease (GBD) Initiative: The GBD was established in 1990 to create tools and measures to quantify the global burden of disease. The GBD Initiative developed the DALY measure and created disability weights to describe the burden of specific diseases on a 0 (healthy) to 1 (dead) scale. There have been four GBD publications: 1990, 2001-2002, 2004, and 2010 (WHO: Global Burden of Disease).
Gross Domestic Product : The value over a specified time period (typically a year) of all finished goods and services produced within a country. The World Health Organization has suggested in the past that researchers assume that averting one DALY is worth 1 or 3 times a country’s per capita GDP (the GDP divided by the size of the country’s population), though WHO is reviewing alternative estimation techniques for considering an appropriate threshold (WHO 2003; Marseille, et al. 2014).
Incremental Cost-Effectiveness Ratio (ICER):
The formula for the incremental cost-effectiveness ratio (ICER) is:
Intervention : The technology, procedure, or health program or service evaluated on a study.
Intervention Impact: Each cost-effectiveness ratio can be assigned a location on the cost-effectiveness plane, illustrated below, based on its incremental cost and health benefit. Interventions that improve health (avert DALYs) are located to the right of the vertical axis. Interventions that increase costs are located above the horizontal axis.
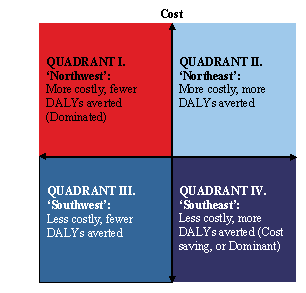
More specifically:
1. An intervention whose ratio is in QUADRANT I (the northwest quadrant) increases costs, but makes health worse (reduces DALYs averted). Ratios in QUADRANT I are sometimes referred to as “dominated”.
2. An intervention whose ratio is in QUADRANT II (the northeast quadrant) increases costs and improves health (increases DALYs averted).
3. An intervention whose ratio is in QUADRANT III (the southwest quadrant) saves money and makes health worse (reduces DALYs averted).
4. Finally, an intervention whose ratio is in QUADRANT IV (the southeast quadrant) improves health and saves money (increases DALYs averted). Ratios in QUADRANT IV are sometimes referred to as “dominant” or “cost saving”.
Millennium Development Goals:
The United Nations established 8 international development goals at the Millennium Summit in 2000. Many international interventions have been implemented in order to achieve these goals (United Nations).
1. To eradicate extreme poverty and hunger.
2. To achieve universal primary education.
3. To promote gender equality.
4. To reduce child mortality.
5. To improve maternal health.
6. To combat HIV/AIDS, malaria, and other diseases.
7. To ensure environmental sustainability.
8. To develop a global partnership for development.
Morbidity rate:
A morbidity rate is typically used to describe disease or illness prevalence in a population at a specific time (Merriam-Webster.com).
Mortality rate:
The mortality rate is typically used to describe death rate in a population a specific time (Merriam-Webster.com).
Perspective:
The viewpoint from which an analysis calculates intervention costs and benefits. Most studies calculate costs from either a societal perspective or a health care payer perspective, meaning that they include all costs and benefits that are relevant to either society or to a health care payer. Studies conducted from a societal perspective typically include costs directly incurred by patients (e.g. copayments), health care payer(s), and spillover costs outside the health sector (e.g. productivity losses resulting from poor health). Studies conducted from a health care payer perspective do not include spillover costs, but do include costs incurred by the government in its role as payer (e.g., Medicare or Medicaid), or other international organizations (e.g. the GAVI Alliance or UNICEF).
Prevention Stage:
Prevention stage refers to the following classifications (Concise Medical Dictionary: Oxford).
Primary: Avoidance of the onset of disease by behavior modification or treatment, such as immunization, promotion of safety equipment use (e.g. seat belts), health education (e.g. anti-smoking campaigns), promotion of improved nutrition and prenatal care.
Secondary: The avoidance or alleviation of disease by early detection and appropriate management. Secondary prevention includes population screening to identify disease in asymptomatic people to enable timely treatment.
Tertiary: Treatment to reduction of complications to mitigate progression of established disease.
Quality Score:
A subjective rating score awarded by reviewers at Tufts Medical Center, who developed and maintain the Registry, ranging from 1 (lowest quality) to 7 (highest quality). Scores reflect the following considerations (in order of importance): 1) whether the authors correctly computed the incremental cost-effectiveness ratios, 2) whether the authors comprehensively characterized the uncertainty of the results (see sensitivity analysis), 3) whether the authors correctly used and explicitly specified the health economic assumptions used in the study (e.g. discount rate, currency, time horizon), and 4) whether the authors appropriately and explicitly estimated the utility weights.
Sensitivity Analysis:
An analysis of the impact on the estimated cost-effectiveness ratio of alternative values for uncertain parameters and assumptions.
• Univariate (One-Way) Sensitivity Analysis: This approach modifies one parameter at a time and records the impact while holding the values for all other parameters equal to their “base case” values.
• Multivariate Sensitivity Analysis: A general term that encompasses any type of sensitivity analysis that changes multiple parameters simultaneously and records the impact on the estimated cost-effectiveness.
• Bounded Sensitivity Analysis: This approach records the impact of changing each parameter to each of its extreme values (upper and lower bounds).
• Probabilistic Sensitivity Analysis: This approach simultaneously selects values randomly from each parameter’s probability distribution (representing the set of plausible values for that parameter), and then estimates the cost-effectiveness ratio corresponding to that set of parameter values. By repeating this process for a large number of iterations, probabilistic sensitivity analysis generates a distribution of simulated cost-effectiveness estimates that corresponds to the joint distribution of model assumptions and parameter values. The resulting distribution of CE ratios can be used to create a cost-effectiveness acceptability curve.
Target Population:
The population(s) eligible for the study intervention.
Time Horizon:
The length of time during which resource use and health effects are measured and summed (Gold et al. 1996).
References:
Center for the Evaluation of Value and Risk in Health. N.d. The Cost-Effectiveness Analysis Registry [Internet]. Institute for Clinical Research and Health Policy Studies, Tufts Medical Center, Boston. Available from: www.cearegistry.org.
Concise Medical Dictionary. Oxford University Press, 2007. Oxford Reference Online. Oxford University Press.
GAVI, the Vaccine Alliance. .
Gold, M.R., J.E. Siegel, L.B. Russell, and M.C. Weinstein, eds. 1996. Cost-Effectiveness in Health and Medicine. New York: Oxford University Press.
Marseille, E., B. Larson; D.S. Kazi, J.G. Kahn; S. Rosen. 2014. Bulletin of the World Health Organization 93:118-124.
Merriam-Webster.com. 2015. www.merriam-webster.com (accessed December 8, 2015).
Murray, C.J. et al. 2012. “Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010.” Lancet 380 (9859): 2197-2223.
United Nations. Millennium Development Goals 2015 and Beyond. www.un.org/millenniumgoals.
World Health Organization. Disability weights, discounting and age weighting of DALYs. WHO. www.who.int/healthinfo/global_burden_disease/daly_disability_weighten/ (accessed December 8, 2015).
World Health Organization. Global Burden of Disease (GBD). WHO. http://www.who.int/healthinfo/global_burden_disease/gbd/en/
World Health Organization. Making Choices in Health: WHO Guide to Cost-Effectiveness Analysis edited by T.T-T. Edejer et al. 2003. Geneva, Switzerland. www.who.int/choice/publications/p_2003_generalised_cea.pdf